This project is led by Dr James Tollitt (Nephrologist) in Salford and is assisted by Andrew Stott (QI Manager) NWKN, Dr Hollie Frances (GP in Oldham) and Iren Szeki (Nephrologist at MFT). The project will also recruit a GP in Tameside.
D- Data driven
R- Risk based renal care
E- Educationally aligned
A- Approachable, Collaborative renal support to Primary Care
M- Medicines optimisation in Manchester
The GM CVD Prevent database describes 217,339 people with CKD in GM. 5219 of these patients are at highest risk of kidney failure ((ACR >=70mg/mmol) but are not on maximised medical therapy. 9761 separate patients are at moderate risk of kidney failure, cardiovascular events and death but are not on maximal therapy (ACR>=30mg/mmol) (unpublished data from CVD Prevent Database). Rapid uptake of medicines optimisation for patients with CKD offers GM a great opportunity to reduce renal disease progression and future cardiovascular events and premature mortality.
Late presentation to renal services can be representative of a failure of the healthcare system whilst also representing room for improvement. Late presentation to a nephrologist is defined as a patient being seen by a kidney service for the first time within 90 days of starting dialysis. According to latest renal registry data 26.2% of patients who commence dialysis at MFT do so as a “late presentation”, 14.1% at NCA. The National average is 19.2% (11). Planned start to renal replacement therapy (RRT) requires patient education, peer support, shared decision making and where possible, preparation for pre-emptive transplantation. Late presentation is associated with increased healthcare costs, increased mortality, and increased morbidity (12–14). Research from Hull et al. suggested that the most important modifiable risk factor associated with late presentation was primary care CKD coding. This remained significant after removing patients who commenced dialysis after an acute kidney injury(12).
Greater Manchester has one of the highest rates of cardiovascular disease and cardiovascular death in the UK (Figure 1)(10). CKD is one of the largest modifiable risk factors for cardiovascular disease.
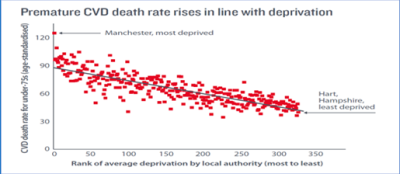
Figure 2 shows variation and hence improvement opportunities in the management and surveillance of CKD in primary care in GM- Whilst all patients with CKD should have their kidney failure risk assessed at least on an annual basis via a blood and urine test, GM CVD Prevent data suggests this only occurs in 18-30% of patients with "coded CKD". Evidence from GM show uptake of medications which mitigate against CKD decline is low- ACE inhibitors or ARBs were shown to reduce renal disease progression over 20 years ago. However, uptake is only 60-70% in GM.
The Northwest Kidney Network (NWKN) has a workstream dedicated to chronic kidney disease (CKD) in Greater Manchester. In March 2024 they applied for transformational funds from Specialised Commissioning North West with agreement from Greater Manchester Integrated care board (ICB) team to undertake a CKD pilot in the GM area. This project is called CKD DREAM.
CKD-DREAM project
D-Data driven approach to CKD.
R-Risk based protocolised Renal care.
E-Educationally aligned.
A-Approachable And collAborative renal support to primary care
M2-Medicines optimisation in Manchester
The aim of this pilot is to:
- Identify patients at risk of CKD and assess their risk of progression.
- Improve management of patients at high risk of progressive CKD.
- Improve the knowledge, confidence and understanding of CKD across all healthcare systems and providers.
- Demonstrate the benefit of closer collaborative and approachable nephrology support to primary care.
This pilot project is aligned to the recommendations of the NHS long term plan that spans prevention, diagnosis, and management of long-term conditions. It is also aligned to the National Renal Service Transformation Programmes recommendations for CKD and the Renal GIRFT recommendations. Our proposed strategy aligns with the objectives of the Core20PLUS5 initiative and seeks to enhance overall health outcomes and reduce health inequalities within the GM ICB. Healthcare does not solely comprise of healthcare professionals and patients. It is a complex interplay of society, economics, politics, and culture. Targets help drive performance and compare locality performances against each other. Local nephrologists building relationships with local healthcare professionals should enable better understanding of the complexities of local issues and ultimately help address the unmet healthcare needs for each locality.
The project is focussed on delivering an accelerated risk-based approach to CKD care underpinned by 4 main aims:
- Identification of patients at risk of CKD in Oldham and Tameside and assess their risk of CKD progression.
- Improve the management of patients in these localities at high risk of progressive CKD.
- Improve the confidence and understanding of CKD across all healthcare systems within Oldham and Tameside so there is a sustainable improvement legacy to the project.
- Demonstrate the benefit of closer collaborative and approachable nephrology support to primary care in these localities.
This project currently being undertaken in GM is in its very early stages, but we will keep you updated with progress at regular intervals.